Abstract
Background: Chronic myelomonocytic leukemia (CMML) is the most common subtype of the rare myelodysplastic/myeloproliferative neoplasms. Some studies have described the possible association with autoimmune disease. With the potential transformation into acute myeloid leukemia, it is known to have an unfavorable prognosis. Previous studies reported TET2, SRSF2, ASXL1, and KRAS/NRAS as the most occurring somatic mutations in CMML. However, the clinical and molecular characteristics of CMML patients in Asia remained fairly unknown.
Materials and Methods: Patients with CMML who were diagnosed in Siriraj Hospital, which is the largest comprehensive cancer center in Thailand, from 2010 to 2020 were identified from the hospital database. Clinical and laboratory data, along with pathological results, were collected from the same database. The results of the 25-gene targeted DNA sequencing panel designed for myeloid neoplasms were also extracted if the results were available. Continuous variables were represented as medians and their associated ranges. Overall survival (OS) was determined using Kaplan-Meier estimator and log-rank test.
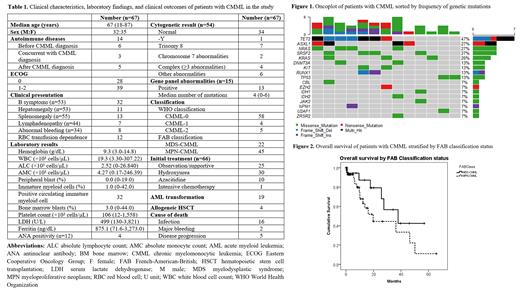
Results: A total of 67 patients with CMML were included in our study. The median age of the cohort was 67 years old with a similar number of male and female patients in the cohort. Thirteen (19.4%) patients were diagnosed with autoimmune diseases, mainly autoimmune hemolytic anemia and immune thrombocytopenic purpura. According to cytogenetic risk for CMML, 35 (64.8%), 6 (11.1%), and 13 (24.1%) patients were classified as low, intermediate, and high risk, respectively. The clinical characteristics and laboratory results of patients were shown in Table 1. For the 15 patients with available molecular results, 13 had at least 1 somatic abnormality with TET2 (46.7%), ASXL1, NRAS, SRSF2 (each 26.7%), and KRAS (20.0%) being the common genetic mutations. The median mutation number was 4 (range, 0-6). The molecular landscape was demonstrated in Figure 1. Overall survival (OS) rates at 1 and 2 years were 74% and 57%, respectively. Patients with MDS-CMML tended to have longer median OS compared to MPN-CMML [37.9 (13.6-62.2) months vs. 19.7 (10.1-29.4) months] but did not reach statistical significance (p=0.124) (Figure 2).
Conclusions: Asian patients with CMML had a considerable amount of associated autoimmune diseases. The genetic mutations contributing to CMML in our cohort also differed from previous reports.
No relevant conflicts of interest to declare.